From Bench to Bedside: Advancements in Understanding and Treating Hypertrophic Cardiomyopathy in Kuwait
Uncovering Novel Mutations and their Associations

Profile Dr. Farida Al-Habib
Academic Background
• حاصلة على درجتَي الماجستير والدكتوراه في طب القلب والأوعية الدموية الإكلينيكي من كلية الطب الملكية للدراسات العليا التابعة لكلية إمبريال كوليدج لندن.
• Fellow of the International College of Angiology in USA.
Professional Experience
• Founder and former director of the Sabah Al-Ahmad Cardiac Center (SACC).
• Former director of the Cardiac Interventional Department at Jaber
Al-Ahmad Armed Forces Hospital.
• Former director of Interventional Cardiac Department at Dar Al Shifa Hospital.
• Consultant Cardiologist at Al-Sabah Hospital.
Professional and International Associations
• Board Member of the Asian-Pacific Heart Foundations Network and
the World Heart Federation.
• Served as Vice-President of the Asian Pacific Heart Foundations Network.
• Member of British cardiac society.
Prizes
• Dr. Al-Habib has been recognized
with prestigious awards, including
“The John Goodwin Award” for Excellence in Cardiology.
Research
Determinants and Outcomes of Hypertrophic Cardiomyopathy in Kuwait; a Clinical, Genetic and Advanced Imaging Study
Dr. Farida Al-Habib
Principle Investigator
Consultant Cardiologist
Al-Sabah Hospital - Kuwait
Professor Sir Magdi Yacoub
The Magdi Yacoub Research Institute
Imperial College of London - UK
Dr. Laila Bastaki
Director of Genetic Center of Kuwait - Kuwait
Dr. Bahia Al-Nafisi
Consultant Radiologist
Consultant Radiologist
Chest Disease Hospital - Kuwait
Introduction
د. فريدة محمد حبيب الحبيب معروفة بمساهماتها في أمراض القلب، و هي صاحبة مسيرة مهنية ممتدة على مدار عقود، تميَّزت بإنجازات رائدة، وتفانٍ في رعاية المرضى. اتسمت رحلة الحبيب بالسعي الدؤوب بحثاً عن المعرفة، والالتزام بتطوير طب القلب والأوعية الدموية. وقد حصلت على مؤ هلات علمية مرموقة، وهي عضو في عديد من المنظمات الطبية الرائدة،
ولها مساهمات بحثية جوهرية، ولذا فإن تأثير الدكتورة الحبيب هو تأثيرٌ ذو صدًى عالمي.
In this exclusive interview, we showcase the results of her latest research, funded by KFAS, on a heart condition called hypertrophic cardiomyopathy (HCM). HCM is an enigmatic disorder, often lurking in the shadows of undiagnosed cases, leading to sudden cardiac death (SCD) in young adults. The aim of this research was to shine a light on this condition, revealing its genetic underpinnings, clinical manifestations, prognosis, and imaging characteristics.
لم يحدِّد البحث طفرات جينية جديدة مرتبطة بتضخم القلب HCM فحسب، بل كشف أيضاً عن ارتباط لم يُبلَغ عنه سابقاً بين تضخم القلب HCM ومتلازمة بروغادا Brugada Syndrome ، مما يُلقي ضوءاً جديداً على تعقيدات أمراض القلب. و هكذا لم تُوسع هذه النتائج المشهدَ الجيني للاعتلال HCM فحسب، بل مهدت الطريقَ أيضاً لتدخلات مبكرة تنقذ حياة المرضى، بما في ذلك غرْسُ مُقوِّم نظم القلب ومزيل الرجفان القابل للغرس (Implantable cardioverter defibrillator ، اختصاراً: المقوِّم
ICD)، لخفض خطر الموت القلبي المفاجئ (Sudden cardiac death) في الأفراد ذوي المخاطر العالية.
What inspired you to embark on this research project, and what are your ultimate goals in terms of its impact on healthcare?
FH: HCM is a hereditary disease caused by a single gene mutation. It follows an autosomal dominant pattern, which means that inheriting just one copy of the mutated gene from a parent is enough to develop the condition. However, not everyone who carries the gene will necessarily show symptoms; this is known as incomplete penetrance, passed down through families where the heart muscle becomes thicker than usual. It is associated and with complex pathophysiology and heterogenic clinical profile, as it involves various changes in how the heart functions and shows up differently in different people, making it challenging to diagnose and treat. It is the leading cause of sudden cardiac death (SCD) in young people. It occurs in one per 500 people and many recent data suggesting a prevalenceof 1 in 200.
ومع ذلك هناك نقص ملحوظ في المعلومات التفصيلية حول هذه الحالة المثيرة للقلق في الأدبيات المنشورة. إذ تظلّ أكثر من
50% من الحالات من دون تشخيص جيني؛ مما يشير إلى احتمال وجود مزيد من الجينات المؤدية إلى هذا المرض. إضافةً إلى ذلك تنقُصنا المعرفة الكافية عن خصائص الحالة وتركيبها الجيني في سكان الكويت، حيث تسود قرابة الدمّ Consanguinity بصورة كبيرة.
Having worked with Professor Sir Magdi Yacoub for 5 years (1991-1996) in London, and being aware of his research network, I was encouraged to seek collaboration with Imperial College London for genetic testing of our patients’ blood samples. However, with the spread of COVID-19 during the first year, handling DNAs was difficult. So, we had to establish our own genetic testing with Dr. Laila Bastaki, the director of the Kuwait Medical Genetic Center (KMGC) Ghanima Al-Ghanem Building. We struggled to acquire the right materials and machines for a type of genetic testing called whole exome sequencing. Eventually, we were successful, ensuring confirmatory inter-observer variability and accuracy.
What are the biggest obstacles you’ve faced during your career in general and this research project in particular and how have you worked to overcome them?
FH: I have worked in different hospitals in various countries throughout my career, starting from Miami Jackson Memorial Hospital and Boston Cambridge Hospital in Boston, to Hammersmith Hospital and Harefield Hospital in London, and ending in Al-Amiri Hospital, Sabah Al-Ahmad Cardiac Center, and Al-Sabah Hospital. This variation in the socioeconomic cultures and health awareness has been a challenge rather than an obstacle. However, the scarcity of biostatisticians in Kuwait has been the biggest obstacle throughout my career, a challenge that was accentuated during this research. The only solution was to attend online courses in biostatistics, commission a StatView programmer, and consult with statistical experts outside Kuwait.
Can you explain the significance of HCM and its prevalence in Kuwait? What prompted you to initiate research specifically focusing on this condition?
FH: عملتُ مع مرضى مصابين بأمراض حرجة في معظم مسيرتي المهنية الطويلة، فتعرّفت على عديد من العائلات التي تعاني تضخم القلب HCM. لتحسين رعايتي الإكلينيكية، كنتُ في حا جة إلى وصف دقيق علمياً لهذا المرض في الكويت. من المعروف أن الأسباب الثانوية لتضخم البطين الأيسر left ventricular hypertrophy (اختصاراًً: التضخم LVH) شائعة لدى مرضى ارتفاع ضغط الدم الكويتيين، لكن السبب الجيني للتضخم LVH غير معروف جيداً.
Our career requires continuous discovery and studies to understand the pathophysiology and characteristics of specific disease in specific population so we can offer optimum management.
What are some of the key methodologies or technologies that were utilized in your research, and how do they contribute to advancing our understanding of heart health?
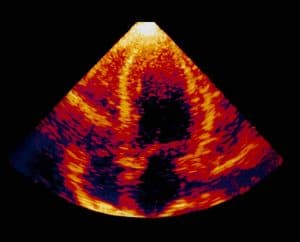
FH: امتدّت الدراسة 36 شهراً، بَدءاً من يناير 2021. وقد التزمنا فيها بأحدث التوصيات العالمية والإرشادات العلمية إلى (2023) التي وضعتها جمعيات القلب الأمريكية والأوروبية، وأجرينا جميع الاختبارات اللازمة وفقاً لذلك. في الزيارة الأولى للمريض، كنا نجمع البيانات الإكلينيكية باستخدام تخطيط القلب الكهربائي ECG، وجهاز هولتر للمراقبة Holter monitoring، وتخطيط صدى القلب Echocardiography، وفحوص التصوير بالرنين المغناطيسي MRI scan ، ونتائج التصوير الإشعاعي. جدولت الزيارات اللاحقة بناء على شدة المرض، واحتفظنا بسجلات لتوثيق حالات دخول المستشفى والأمراض المصاحبة والمضاعفات.
قدّم لنا استخدام تخطيط صدى القلب والتصوير بالرنين المغناطيسي للقلب في جميع الحالات (156)، بالإضافة إلى استخدام التصوير بالرنين المغناطيسي المعزز بالتباين بالغادولينيوم Gadolinium contrast MRI، بياناتٍ موسعةً عن ثخانة الجدار وموقع الثخانة (الجدران الأمامية والخلفية للحاجز Septum والقمة Apex) وعلاقته بتليف عضلة القلب Myocardial fibrosis. وفي حين أن الأدبيات المنشورة من الدراسات الجينية المتطورة السابقة تشير إلى أن نحو 50% من الحالات تحمل الجينات ذات الصلة، إلا أننا قد وثّقنا أنّ 58.7% من مرضانا يحملون الجين المسبِّب للمرض.
What significant genetic discovery have you made in your research, particularly concerning HCM within consanguineous families, and what implications does this finding have for the broader understanding of HCM and genetic research?
FH: We’ve identified a novel genetic mutation, which are variants or different forms of a gene, in the ALPK3 gene inherited from both parents (homozygous variant). This mutation causes the addition of a different amino acid, known scientifically as a missense disease-causing mutation, leading to the emergence of the disease in a family where consanguineous marriage prevails, and individuals have recessive HCM. This means that the disease only manifests when the individual inherits two non-dominant genes.
The discovery of new, rarely studied but important genes like TRIM63, BSCN, and ALPK3 in patients with hypertrophic obstructive cardiomyopathy (HOCM) is noteworthy. This has been reported in two children who suffered SCD before their teenage years. Fortunately, our patient with homozygous ALKP3 was in his forties with positive consanguinity. The presence of myocardial fibrosisin the MRI data had significant effecton clinical manifestation of HCM as well as prognosis.
This underscores the necessity of broadening genomic research to include less-explored consanguineous populations. Doing so will help unravel the effects of new biallelic variants and recessive genes on the HCM phenotype, shedding light on crucial aspects of this condition.

How do these findings contribute to our understanding of cardiac diseases and the potential for early interventions to prevent SCD?
FH: Through our research, we have not only identified novel genetic mutations associated with HCM but also uncovered a previously unreported
association between HCM and Brugada Syndrome, shedding new light on the complexities of cardiac diseases. Both diseases cause ventricular tachycardia.
We also looked at a new association between patients with HCM and Brugada Syndrome. The latter is a rare genetic disease with distinctive ECG characteristics. It is responsible for 20% of cases of sudden death due to serious ventricular arrhythmias in healthy individuals with a structurally normal heart, and 4% of all causes of sudden death. Our findings have not only expanded the genetic landscape of HCM but have also paved the way for early interventions, including ICD implantation, to mitigate the risk of SCD in high-risk individuals. This association has not been reported previously and warrants further studies using new models and tools in biomedicine, as both diseases are important causes of SCD. This result underscores the need to address a rarely reported gene and peculiar clinical characteristics. This study has generated a substantial database for patients with HCM, which can be used in the future by all doctors in Kuwait. By explaining the determinants and outcomes of HCM in Kuwait, our research not only fills a critical gap in the literature but also serves as a foundation for future studies and initiatives aimed at enhancing early detection and management of this life-threatening condition, I hope we can establish a nationwide database to track all HCM cases, which will enhance the management of the patients and encourage future scientific research.
How did the collaboration between MOH/KFAS in Kuwait and Imperial College London enhances the scope and potential outcomes of your research?
FH: Actually, the collaboration was in the first year only. Amidst the COVID-19 outbreak, I personally transported the DNA samples to the laboratories of Professor Yacoub. Later, and despite the challenges, we managed to acquire all necessary reagents and exomes at KMGC.
The team extends his gratitude to Sir Magdi Yacoub for his guidance and discussions. More importantly, I have attended Professor Magdi’s surgical operations on HCM patients. He is a pioneer in this type of surgery, which is rare worldwide and relatively new. Surgical myectomy involves reducing the size of the heart by removing hypertrophied segments of the myocardium. It was essential for me to observe these procedures firsthand so that I can explain them thoroughly to my patients. Additionally, I have discussed the introduction of this important surgery to the Kuwaiti surgical team with Dr. Jamal Al-Fadhli, the director of Chest Disease Hospital. He expressed great interest in initiating training and establishing this surgery in Kuwait rather than sending patients abroad.
Could you elaborate on the multidisciplinary approach utilized in your research project? How does this collaborative approach improve patient care and treatment outcomes?
FH: Our multidisciplinary approach, involving cardiologists, radiologists, pediatricians, and genetic specialists, has been pivotal in unraveling the mysteries of HCM and providing comprehensive care to our patients in Kuwait. The cardiologist would refer potential cases to me, and I meticulously evaluated them to rule out any secondary causes of ventricular hypertrophy through clinical assessments, including ECGs and Holter monitoring. Simultaneously, Dr. Bahia Al-Nafisi and her team conducted MRI scans, and Dr. Laila Bastaki and her team undertook the genetic characterization of all patients and their families.
We held regular auditing meetings to validate all diagnoses periodically, as well as sessions with patients, their siblings, and relatives after a comprehensive analysis of all data. These meetings aimed to explain various treatment options and prognosis. Additionally, we referred children to pediatricians when necessary.
Could you share any memorable moments or breakthroughs that have occurred during the course of your research?
FH: In one of our audit meetings, we uncovered a new relationship between HCM and Brugada Syndrome, another cause of SCD, which had not been reported before. This discovery stirred a range of emotions in me— excitement at revealing this previously unknown connection between HCM and Brugada Syndrom, alongside feelings of sadness and distress when discussing the implications with the parents of younger siblings.
For example, I vividly recall a case involving a 6-year-old asymptomatic boy. It was challenging to convey to the family the necessity of undergoing investigations such as the Flecainide test to induced Burgada ECGs and subsequent implantation of an intra-cardiac device to prevent sudden death. This emotional experience demanded delicate communication, employing reserved language and speaking softly to ensure they comprehended the diagnosis, treatment options, and prognosis. A great psychological support to both the family and the child was needed.
Could you expand on the importance of your research findings concerning the patient profile of HCM, especially within the context of the Kuwaiti population, where such data was previously unavailable?
FH: This research has revealed a new group of patients at risk of sudden death due to serious arrhythmias, allowing us to proactively protect them by implanting ICDs, often at a young age.
Likewise, identifying myocardial fibrosis through late gadolinium enhancement MRI, has significantly influenced patient therapy decisions and facilitated the selection of more aggressive treatment modalities like surgical myectomy. While this approach is relatively novel and performed in only a few centers, we have sent seven patients abroad for this procedure, and their outcomes have been very promising. Consequently, this research lays a solid foundation for introducing this surgery in Kuwait, potentially saving lives, particularly in severe cases.
In addition, the research offers insights into addressing the issue of consanguineous marriages within affected families in Kuwait, which heightens the risk of having affected children. This research could enhance public awareness of early discovery of the disease and early treatment before any tragic event.
Any final words?
FH: FH: I am delighted to share these results. Many thanks to the Kuwait Foundation of the Advancement of Sciences (KFAS) and the Research and Technology Directorate for their exceptional cooperation and professionalism. I’m grateful to Professor Sir Magdi Yacoub and Dr. Ameenah Farhan, the General Director of KFAS, for their guidance. Special appreciation to Dr. Laila Bastaki, Dr. Bahia Al-Nafisi, Sobhi Hussain, and Ahmad Salim from the MOH.
The Outcomes
• The outcome of this research lead to establishing a Center of Excellence in Kuwait for the clinical and therapeutic management of patients with inherited cardiomyopathies. Patients in the project had multidisciplinary approach that included collaborative work with cardiologists, radiologists, pediatricians, and genetic specialists, among others.
• The research team determined the genetic basis of the disease in the Kuwaiti population by including 56 non-Kuwaiti patients to the cohort of 100 Kuwaiti patients, making a total of 156. This cohort represents the diversity of the Kuwaiti population. We identified associated mutations and related genotype to phenotype. We also detected 3 new novel genes, namely TRIM63, BSCN, and ALPK3 that are rarely described in literature.
• The research discovered a new relationship between HCM and Brugada Syndrome, which has not previously been reported.
• Potential determinants examined included genotype, extent and location of hypertrophy as determined by echo and MRI, and extent of fibrosis as determined by late gadolinium enhancement MRI.
• The team also studied extended cardiac myectomy in a sub-cohort of 7 Kuwaiti patients with obstructed conditions who underwent surgical intervention this year (2024).