website_taqadom
-
بيولوجيا

ثورة في رعاية مرضى السرطان
بروفايل الدكتور سالم حمد الشمري المؤهلات الأكاديمية: • بكالوريوس الطب والجراحة (B.M.B.CH)، جامعة الكويت، 1987. • زمالة الكلية الملكية للأطباء في كندا (FRCPC)، الطب / أمراض الدم – غرب أونتاريو، كندا، 1994. • زمالة في زراعة نخاع العظام – مركز…
-
بيولوجيا

من البحث إلى العلاج: رحـلة الدكـتور سـالم الشمـري وتحويل الطب تحويلًا جذريًّا
لعقود من الزمن، اعتمد علاج السرطان على نهج موحد، غالبًا ما يستخدم العلاج الكيماوي الشرس ذا الآثار الجانبية الشديدة. ومع ذلك، فإن التطورات في الطب الدقيق تعيد تشكيل علم الأورام، مما يتيح العلاجات المصممة خصيصًا للمرضى كأفراد. يقود هذا التحول…
-
ألزهايمر
الريادة في تصميم المباني المستدامة: دروس مستفادة من أبحاث برج الحمراء
برج الحمراء هو أطول برج خرساني منحني في العالم، إذ يبلغ ارتفاعه نحو 414 متراً. وهو لا يعتبر تحفة معمارية فحسب، بل ومنارة للأبحاث المبتكرة في مجال مراقبة صحة وسلامة المباني. إذ موّلت مؤسسة الكويت للتقدم العلمي المشروع البحثي «نمذجة…
-
أعمال

ابتكار معالجة المياه باستخدام الموارد المحلية
لم يكن عبدالرحمن الصليلي يتوقع أن يبني مسيرته البحثية حول المياه؛ فبعد أن قاده حبه للرياضيات إلى الحصول على درجة البكالوريوس والماجستير في الهندسة المدنية من جامعة الكويت، حصل بعد ذلك على منحة دراسية للحصول على درجة الدكتوراه في جامعة…
-
أعمال

غرفة لذيذة: إعادة هندسة الآيس كريم الكلاسيكي لمستقبل أكثر صحة
تؤثر المعدلات المرتفعة من الأمراض الأيضية، مثل مرض السكري من النوع الثاني، على الناس في جميع أنحاء العالم، والكويت ليست استثناءً. قالت الدكتورة إباء العزيري، رئيسة قسم الطب في معهد دسمان للسكري: «تبلغ نسبة انتشار مرض السكري من النوع الثاني…
-
أصنع معداتك الفلكية بنفسك

معهد دسمان للسكري يفوز بجائزة نجمة السلامة
حصل قسم الأشعة التشخيصية في معهد دسمان للسكري DDI- أحد المراكز التابعة لمؤسسة الكويت للتقدم العلمي -على جائزة «نجمة السلامة» للعام 2023، وهي جائزة تمنحها وزارة الصحة في الكويت؛ تكريمًا للجهود الاستثنائية في تعزيز سلامة المرضى، والالتزام بمعايير الجودة العالمية.…
-
أخبار

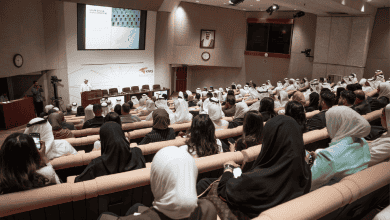
شهر العلوم 2024 في الكويت… رحلة عبر الابتكار والاكتشاف
أطلقت مؤسسة الكويت للتقدم العلمي، ومراكزها وشركاؤها، شهرَ العلوم 2024 في الكويت (SciMik). أُقيم شهر العلوم – هذا العام – في الفترة من 14 نوفمبر إلى 12 ديسمبر، وضم ورش عمل تفاعلية، ومعارض، ومحاضرات، وأنشطة عائلية، وفعاليات ميدانية، تستكشف موضوعات…
-
أخبار

ربط العلوم بالسياسات من أجل مستقبل الرعاية الصحية في الكويت
عقد «برنامج الكويت» مع كلية لندن للاقتصاد (LSE) مؤتمره للعام 2024 في الكويت، والذي سلط الضوء على أهمية الابتكار في مجال الرعاية الصحية وإصلاح السياسات. وبرعاية مؤسسة الكويت للتقدم العلمي، تضمن الحدث مناقشات بناءة حول تكنولوجيا الرعاية الصحية والعوامل الاجتماعية…
-
جائزة نوبل

الاحتفال بعام من التقدم والوعود
مع اقتراب عام 2024 من نهايته، تعتز مؤسسة الكويت للتقدم العلمي بذكرى عام اتسم بالنمو والابتكار والمساهمات المؤثرة. فمن رعاية المواهب المحلية إلى تعزيز التعاون العالمي، أثبتت مؤسسة الكويت للتقدم العلمي مرة أخرى التزامها الراسخ بتقدم العلوم وتحفيز الابتكار وإلهام…
-
ابتكار

المستقبل غيرُ الجراحي لمراقبة الصحة: رحلة دينا القتابي في الهندسة والطب
“إن إنفيزيبلز Invisibles هي طريقة غير باضعةٍ لتتبُّع الصحة. تتمتع إي كيو-راديو EQ-Radio بالقدرة على تحويل البيئات بناءً على مزاج الشخص” دينا القتابي. تستطيع المهندسة الكهربائية دينا القتابي أن تقول بحق إنها تُحدِث ثورة في الطب بصفتها أستاذة دكتورة ثوان ونيكول…